If the cornea progresses and contacts cannot be tolerated some form of surgery may become necessary. With keratoconus, you are not a suitable candidate for LASIK surgery. But there are several other options that include INTACS, Collagen crosslinking (CXL), Corneal transplant surgery. Make your appointment today. Come see the Manhattan Eye Doctors & Specialists and meet a New York City optometrist Dr. Saba Khodadadian and ophthalmologist Dr. Richard L. Deluca.
Keratoconus
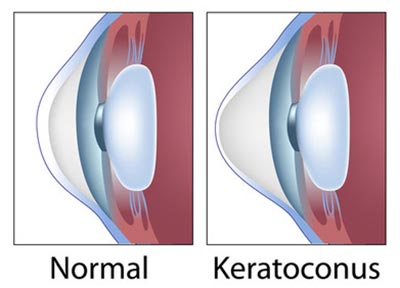 Keratoconus is a disorder that occurs when the front part of your eye, round and smooth when healthy, becomes thin and abnormal, taking on more of a conical shape. Since the round shape of your eye is meant to help focus light, keratoconus forces the light to be angled improperly through the cornea and onto the retina.
Keratoconus is a disorder that occurs when the front part of your eye, round and smooth when healthy, becomes thin and abnormal, taking on more of a conical shape. Since the round shape of your eye is meant to help focus light, keratoconus forces the light to be angled improperly through the cornea and onto the retina.
The main result from the condition is distorted vision. Because it’s the very shape of the eyeball that’s irregular, eyeglasses or lenses will only help in the early stages of the disease. You’ll most likely need special lenses as this uncommon disease progresses.
If you are having any abnormal visual symptoms, you should always be evaluated with a thorough consultation and examination by a ophthalmologist or optometrist in NYC for an accurate diagnosis and treatment plan as it may be a symptom or sign of a serious illness or condition.
Primary Symptoms
Keratoconus often is considered a pediatric eye malady, as symptoms usually present sometime between the teens and the early twenties. The symptoms continue to persist over a 10- to 20-year period. The most common symptoms include:
- Distorted vision, including mild blurriness
- A sensitivity to lights and glare
- Mild nearsightedness
- Astigmatism
- Difficulty driving, typing, watching television or reading
- Frequent changes in prescription over the years
- Discomfort when attempting to wear contact lenses
- Cloudy vision
If you are having any visual abnormalities you should always be evaluated with a thorough consultation and examination by a ophthalmologist or optometrist in NYC for an accurate diagnosis and treatment plan as it may be a symptom or sign of a serious illness or condition.
Typical Progression
This eye disease often starts in one eye. While it may spread to the other eye, each eye reacts differently to the changes. Most people notice that the disease stops progressing in their 30s. If you are diagnosed at a particularly young age, you are more likely to need surgical intervention.
As time progresses, the disease may stop and re-start without warning. The cornea problems usually continue, as the bulge grows and the cone-shape becomes more pronounced. There is a possibility that the cone shape, which the eye isn’t built to support, eventually gives under the pressure, and a small crack occurs. If this happens, you’ll experience some swelling as your eye heals. This could last for weeks or even months. Beyond drops for pain relief, there is not much that can be done until your eye heals.
Causes of Keratoconus
Men and women suffer equally from this disease. There appears to be no concrete genetic factors; only about 13 to 15 percent of those diagnosed with keratoconus have a family member with the same disease. Despite the piles of research, no clear, confirmed cause of keratoconus has been found. However, the disease has been associated with:
- Eye injury, often caused by repeated, vigorous rubbing of the eyes
- Other eye diseases such as retinitis pigmentosa, retinopathy of prematurity and vernal keratoconjunctivitis
- Diseases that impact the entire body, such as Leber’s congenital amaurosis, Ehlers-Danlos syndrome, Down syndrome and osteogenesis imperfecta
Testing and Diagnosis
Diagnosis often is made by a cornea specialist because the regular slit-lamp evaluation performed during a routine eye exam with your ophthalmologist may not in fact reveal any changes in your cornea. Instead, the tests performed to check the curvature of your cornea may include:
- Computerized videokeratography, which takes pictures of your cornea so a map can be made of the surface while also measuring the thickness of your cornea
- Keratometry that uses light and reflection to determine the curvature of your cornea
- Eye refraction that relies on special equipment to check for vision problems
- Slit-lamp examination, which is the most common test and involves a beam of light directed into your eye so the doctor can see your cornea and retina using a small microscope
These tests give your doctor important clues that can point to a proper diagnosis, including:
- Corneal thinning
- An iron-colored ring all around the cone, also known as Fleischer’s ring
- Stress lines caused by the change in cornea shape, also called Vogt’s striae
- Scars at the top of the cone of your eye, also called apical scarring
At Manhattan Eye Doctors & Specialists, a top rated optometrist in New York City, optometry specialist Dr. Khodadadian and Dr. Richard L. Deluca, an opthamologist in NYC offers varying eye care treatments from simple vision test to the most complex eye surgeries.
Treatment Options
Contact lenses can be used to correct astigmatism and mild near-sightedness that can occur as secondary issues to keratoconus, at least in the early stages. The traditional treatments for keratoconus include:
- Hard or rigid contact lenses for keratoconus have been a go-to solution for doctors trying to correct vision. While they can be a little uncomfortable at first for new users, your eyes will adjust.
- SynergEyes hybrid contact lenses are fairly new to the market. They are a unique combination of hard and soft lenses, with a rigid center and soft edges. They were made to be a bit more comfortable for those who couldn’t tolerate hard lenses while giving eyes the support they need.
- Soft contact lenses or eyeglasses are always an option, but they usually require you to update your prescription regularly to keep up with the changing shape of your cornea.
- Because patients often struggle with hard, gas permeable lenses, your doctor may suggest that you “piggyback” lenses, that is, wear a soft lens on your eye, with a hard lens on top for added support.
- Scleral lenses are used by people who cannot tolerate hard lenses at all. Instead, these lenses arched so that the edges rest on the whites of your eye and the top arcs over your cornea without touching it.
Complications
As your eye shape changes, there can be discomfort with some contact lenses, which can stem from abrasions from the contact lens moving unevenly over the abnormally shaped cornea, leading to light sensitivity. Dry eye can come from your eye’s struggle to keep the eye lubricated with its new shape. It makes wearing contact lenses uncomfortable.
Excessive rubbing from contacts can leave a small scar on the cornea, which may lead your doctor to perform a minor surgery called phototherapeutic keratectomy (PTK) or nebulectomy, during which the scar tissue is removed for your comfort.
Surgical Interventions
Ultimately, some form of surgery may become necessary if the cornea progresses in its shape-changing until it is so steep that contacts cannot be tolerated at all. With keratoconus, however, you are not a suitable candidate for LASIK surgery. You have several other options that include:
- INTACS are described as arc-like and plastic. These pieces are inserted into the center of the cornea to flatten it, thereby making the eye more contact lens-tolerant.
- Collagen crosslinking (CXL) with UVA is a complex surgery that involves removing the topmost layer of your cornea, adding vitamin drops and then exposing the eye to a special UV lamp that helps the cornea fibers multiply, strengthening the cornea. Full recovery can take several months.
- Corneal transplant surgery is the last resort for most doctors. As the name suggests, your cornea would be removed and replaced with a healthy, normal-shaped cornea. This surgery has a long recovery time, a year or more in some cases, before you start seeing better.
If you are having any abnormal visual symptoms, you should always be evaluated with a thorough consultation and examination by a ophthalmologist or optometrist in NYC for an accurate diagnosis and treatment plan as it may be a symptom or sign of a serious illness or condition.
Important Reminder: This information is only intended to provide guidance, not a definitive medical advice. Please consult eye doctor about your specific condition. Only a trained, experienced board certified eye doctor can determine an accurate diagnosis and proper treatment.
Do you have any questions about Keratoconus Surgical Treatment in NYC? Would you like to schedule an appointment with Manhattan ophthalmologist Dr. Richard L. Deluca, optometrist Dr. Saba Khodadadian of Manhattan Eye Doctors & Specialists? Please contact our office for consultation with New York eye doctor.
Dr. Saba Khodadadian, Optometrist (NYC Eye Doctor)
New York, NY 10028
(Between Madison Ave & Park Ave)
☎ (212) 533-4821


